Kay points:
- Trauma isn’t the event; trauma is our parts reacting to the event.
- Understanding this distinction is crucial when you aim to support someone with trauma.
- Loved ones may assist by listening, respecting boundaries, and being there.
- Do not use quick answers or shut-down statements that silence or humiliate parts.
- It also includes self-care along with the identification of secondary trauma.
- Professional help, including Internal Family Systems (IFS), can guide deep healing.
What is Trauma Anyway?
Whenever trauma is discussed, most people’s minds go directly to the incident itself—injury, accident, violence, abuse, disaster. But trauma’s less about why it happened but why it lasts. It’s the aspects of our being that instil fear, shame, or helplessness beyond the incident itself.
Statistics also show that about 70% of adults will have at least one traumatic event in their lifetime, and about 20% will go on to develop symptoms characteristic of PTSD. But statistics don’t tell all. Trauma could reside in the body and the spirit on subtle levels: nightmares, flash panic attacks, freezing up, blaming yourself, or not being able to relate to others.
In IFS (Internal Family Systems), trauma presents itself as something parts carry—usually exiles who carry the wound, protectors who keep it safe at all costs, managers who attempt to keep life on track. What this lens presents for me is the way trauma reactions aren’t weakness but survival mechanisms.
Common Ways Trauma Reveals Itself
Each person’s system responds individually. There are some universal patterns:
- Nightmares or flashbacks as if they are reliving the trauma.
- Avoiding situations, people, or places that might remind them of the event.
- Hypervigilance—you’re on the alert all the time.
- Blaming or shaming oneself, even though logically they recognise it was not their fault.
- Dissociation, where a part of them “checks out” to survive overwhelming feelings.
- Feelings of numbness, so happiness and intimacy seem distant.
These reactions might sound frightening on the surface, but in the language of IFS, they make perfect sense: they are protectors simply trying their best to safeguard the system.
How You May Help the Person You Love
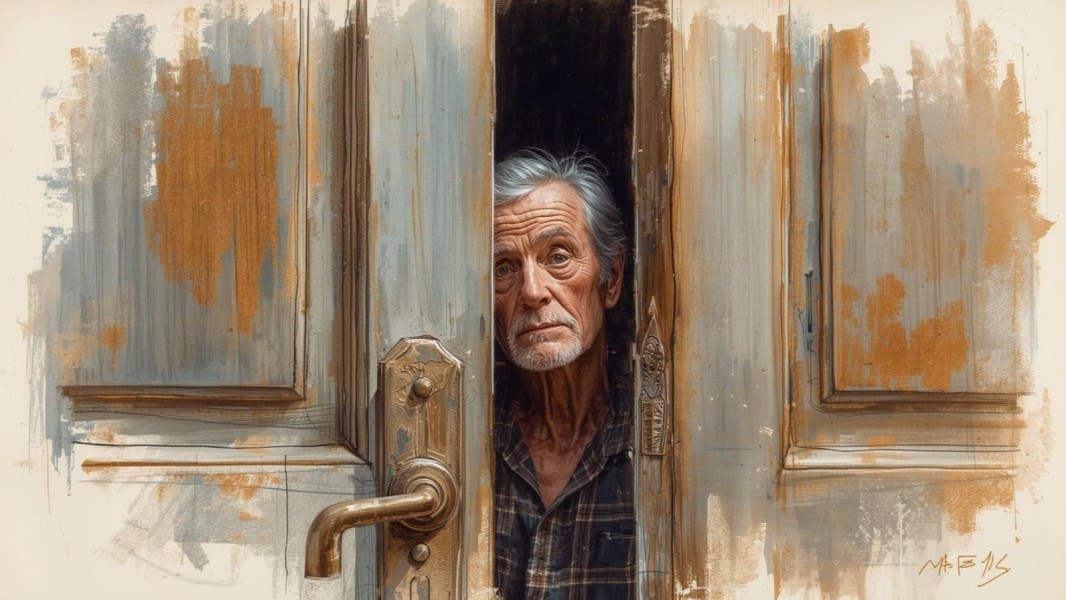
It’s intimidating being around someone who has trauma. Sometimes, a part of you wants their suffering to disappear, but the truth is, it won’t. What you can do instead is create a space where their system might feel less vulnerable.
1. Listen Without Correcting
Active listening is powerful. Instead of rushing into solutions, take a moment to reflect on what you hear. Comments like “I’m with you” or “Thanks for trusting me” reassure safeguarded parts that they don’t have to protect against minimisation or disbelief.
2. Respect Their Space
Trauma causes people to feel unsafe in their environments as well as in their own skin. Always obtain permission before touching them, even for as little as a hug. Emotional space is also a factor—don’t make them disclose details they don’t want to share.
3. Be Present, Not Perfect
They don’t require the perfect words. They only need you to remain. Seated in silence, providing soft comfort, or just participating in daily life may bring their system the memory it’s not alone.
4. Be Patient
Depending on the sections being worked on, different ones may be required at other times. Some days, they may crave being around people, while on other days, they may retreat. Patience asserts you’re not imposing their recovery on your schedule.
5. Extend Assistance on the Fundamentals
Trauma may complicate concentration as well as everyday life. Preparing a meal, assisting with errands, or simply reminding them of appointments may alleviate some of the burden on them.
What Not to Do
Even when intended well, certain comments will shut down parts or trigger shame. Don’t ever do something like:
- “It wasn’t so bad.”
- “Just move on.“
- “Put on a bright face.”
- “I feel the way you feel.”
These reactions, as well-meaning as they may be, discount or override the internal reality of the traumatised parts. Better options include simple grounding statements, such as “I hear you.“ “I’m present when you need me.“ “You’re not alone.”
Don’t Forget About Caring for Yourself
Accompanying someone through trauma carries its own burden. Secondary trauma is no illusion—you may feel drained, anxious, or even incapacitated yourself. Keep in mind: you can only be there for someone else when you’re taking care of yourself as well. Therapy, support groups, or even basic routines such as rest and exercise can help you remain steady.
When Professional Help Matters
Sometimes the symptoms clear up spontaneously after several months. However, where distress persists for months or where daily existence, as well as social relationships, come under threat, professional help may be beneficial.
Interventions like EMDR, trauma-focused CBT, or somatic interventions like yoga and meditation have benefited. What Internal Family Systems contributes as an additional crucial dimension is the recognition that, rather than attempting to eliminate or resist trauma symptoms, it enables individuals to access the parts within themselves that hold the suffering and access the healing inherent within.
An IFS therapist guides the client into befriending their protectors, trusting their exiles, and surrendering ever-increasing burdens. Healing removes the past—it doesn’t erase it—it changes the relationship to it.
Conclusion
The Results
You can’t carry their trauma for them, but you can hold their side. You can allow their parts to feel seen, held in dignified regard, not alone. Sometimes the best thing you can provide is saying, “I am here, and I am not leaving.”
If you or someone you love is traumatised, know this: help is on the way. There’s healing available. There’s not an ounce of us too broken to lend a hand.